Abstract

Background
β-globin gene transfer into hematopoietic stem cells (HSCs) may reduce or eliminate the acute symptoms and long-term complications of sickle cell disease (SCD). LentiGlobin Drug Product (DP) contains autologous CD34+ cells transduced with the betibeglogene darolentivec (BB305) lentiviral vector, which encodes a β-globin with a single point mutation (AT87Q) designed to confer anti-sickling properties similar to γ-globin. HGB-206 is a multi-center, phase 1/2 safety and efficacy study of LentiGlobin DP in adults with severe SCD. In 2016, the HGB-206 protocol was modified to increase DP vector copy number (VCN), require pre-harvest transfusions, increase target busulfan levels, and explore the use of plerixafor for mobilization and apheresis for cell collection. We present new data from the initial 7 patients (group A) and initial data from 2 newly treated patients (group B, with increased DP VCN and pre-harvest transfusions). Results from exploratory plerixafor-mediated HSC mobilization will be reported separately.
Methods
Patients (≥18 years of age) with severe SCD (history of recurrent vaso-occlusive crisis [VOC], acute chest syndrome, stroke, or tricuspid regurgitant jet velocity of >2.5 m/s) were screened for eligibility. For group B, at least 2 months of regular transfusions (target Hb 10-12 g/dL and target HbS <30%) were initiated. Following bone marrow harvest (BMH), autologous CD34+ cells were transduced with the BB305 vector. Subjects underwent fully myeloablative conditioning prior to infusion of the transduced cells. After infusion, patients were monitored for adverse events (AEs), engraftment, vector copy number (VCN), HbAT87Q expression, and laboratory and clinical parameters.
Results
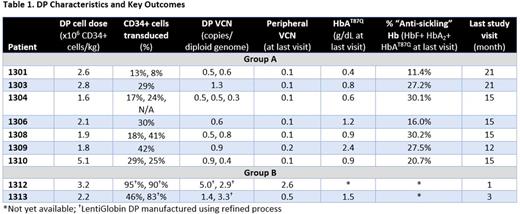
As of July 21, 2017, 9 patients with severe SCD (median age 26 [range 18-42] years) have received LentiGlobin DP. All successfully underwent BMH (median 2 harvests, range 1-3). Eighteen grade 3 AEs in 6 patients were attributed to BMH: pain (12 events), anemia (3 events) and VOC (3 events). Table 1 summarizes DP characteristics and lab results. The median cell dose for group A patients was 2.1 x 106 CD34+ cells/kg, median DP VCN was 0.6 copies/diploid genome, and 8%-42% CD34+ cells were transduced. In group B patients, DP VCNs were 1.4/3.3 and 2.9/5.0 (2 DP lots per patient), DP cell doses were 2.2 and 3.2 x 106 CD34+ cells/kg, and 46%-95% of CD34+ cells were transduced. Median time to neutrophil engraftment (ANC ≥ 500) was 22 days (range 17-29) in group A and 28 days in group B. Median post-infusion follow-up as of June 2, 2017 was 18.3 (14.9-23.8) months in group A. Patients in group B had 1.7 and 5.6 months follow-up as of July 21, 2017. The toxicity profile observed from start of conditioning to latest follow-up was consistent with myeloablative conditioning with single-agent busulfan. To date, there have been no DP-related ≥ grade 3 AEs. Sixteen SAEs in 7 patients have been reported post DP-infusion, including 2 episodes of grade 4 bacteremia, 2 episodes of grade 3 pyrexia, and single episodes of grade 3 long QT syndrome, fever, influenza, wrist fracture, osteonecrosis, pain, iron overload, pulmonary mass, vomiting, diarrhea, and drug dependence.
In group A, median VCN in peripheral blood was 0.1 (0.1-0.2) copies/genome and median HbAT87Q level was 0.9 g/dL (0.4-2.4 g/dL) at last measurement. Patients experiencing multiple VOCs prior to study entry (n=6; median 4, range 2-28 VOCs annually) have had numerically fewer VOCs since LentiGlobin DP infusion (median annualized frequency 1, range 0-24, 14%-100% reduction).
In group B, the marked increases in DP VCN have corresponded to higher early VCNs in peripheral blood, with VCNs in patients 1302 and 1303 of 2.6 and 0.5 at month 1 and month 3, respectively. An additional 8 patients have been enrolled in HGB-206 as of July 21, 2017 but have not yet received DP. Initial data, including mobilization results and DP characteristics, for these patients will be presented.
Conclusions
Early results from 2 patients treated under a modified protocol with LentiGlobin DP manufactured under a refined process demonstrate both higher DP VCN and higher peripheral VCN after transplant. Engraftment times in group B are comparable with group A, and no unexpected AEs have occurred to date. Additional study data should demonstrate whether improvements in LentiGlobin gene therapy will provide consistent clinical benefit to patients with severe SCD.
Kanter: Sancillo: Research Funding; GBT: Research Funding; Pfizer: Research Funding; Apopharma: Research Funding; MUSC: Other: The site PI for sponsored research conducted at MUSC who receives funds from: Novartis, bluebird bio, GBT, Sancillo, Apopharma, Pfizer; AstraZeneca: Membership on an entity's Board of Directors or advisory committees; NHLBI (sickle cell disease research advisory committee): Membership on an entity's Board of Directors or advisory committees, Research Funding; Bluebird Bio: Membership on an entity's Board of Directors or advisory committees, Research Funding; Novartis: Membership on an entity's Board of Directors or advisory committees, Research Funding; American Society of Hematology (Sickle Cell Disease Guideline Panel): Membership on an entity's Board of Directors or advisory committees. Walters: bluebird bio: Research Funding; Sangamo Therapeutics: Consultancy; AllCells, Inc: Other: Medical Director; ViaCord Processing Lab: Other: Medical Director. Kwiatkowski: Agios: Consultancy, Honoraria; Bluebird Bio: Research Funding; Apopharma: Research Funding; Ionis: Consultancy, Honoraria; Novartis: Research Funding. von Kalle: bluebird bio: Consultancy; GeneWerk: Equity Ownership. Joseney-Antoine: bluebird bio: Employment, Equity Ownership. Pierciey: bluebird bio: Employment. Shi: bluebird bio: Employment, Equity Ownership. Asmal: bluebird bio: Employment, Equity Ownership. Thompson: Celgene: Consultancy, Research Funding; Novartis: Consultancy, Research Funding; Baxalta: Research Funding; bluebird bio: Consultancy, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal